The endocrine system comprises a network of glands and hormones that are key regulators of bodily functions (growth, metabolism, reproduction), development, the response to stress, mood, and many other processes.
This module focuses on the drugs that are available to treat diseases that are caused by defects in hormone signalling pathways. These might include hormone replacements for conditions like diabetes, hypothyroidism, adrenal insufficiency or growth hormone deficiency, or drugs that antagonise pathways that are overactive (hyperthroidism e.g., Grave’s disease, functioning pituitary adenomas that secrete high levels of certain hormones such as prolactin, ACTH/Cushing’s disease, TSH/hyperthyroidism, growth hormone/acromegaly). The principal goal of treatments for endocrine system disorders is to re-establish normal hormonal regulation and restore physiological functions to more appropriate levels.
If you have relevant content you are willing to share, we would appreciate your contribution. Contact admin@pharmacologyeducation.org, or complete the webform on the Contribute to the Project page.
Antihyperglycemics (1)- oral
Antihyperglycemic medications are used for glycemic control. Maintaining appropriate blood glucose levels in patients with hyperglycemia is important for minimizing the risk of acute symptoms, long-term complications, and mortality. There are many physiological causes of hyperglycemia, so multi-drug regimens may be required to control blood glucose levels.
Currently, there are 7 classes of oral antihyperglycemics.
Biguanides: metformin
Metformin is considered first line for treatment of type II diabetes mellitus. This oral medication is the only antihyperglycemic with evidence for decreasing premature mortality independent from glycemic control. Metformin acts as an insulin sensitizer by reducing hepatic glucose production. Metformin is contraindicated in patients with heart failure and a creatinine clearance <30 mL/min due to a risk of life-threatening lactic acidosis.
Sulfonylureas: glyburide (glibenclamide), glipizide, glimepiride
Sulfonylureas increase insulin secretion by stimulating pancreatic beta cells. Beta cells may become sensitized to these medications over time, eventually resulting in failure. Sulfonylureas may cause hypoglycemia, so dose initiation or titration should be done conservatively. Due to the risk of drug accumulation in patients with renal impairment, glyburide is not recommended, and glipizide/glimepiride should be used with caution. These drugs are associated with weight gain and an increased risk of cardiovascular death in patients with coronary artery disease.
Sodium-glucose cotransporter-2 (SGLT-2) inhibitors: empagliflozin, canagliflozin, dapagliflozin
SGLT-2 inhibitors promote glucose excretion by blocking its reabsorption in the kidney. In addition to lowering blood glucose, this class may also promote weight loss and cardiovascular benefits. The use of these medications is limited by risks, including genital infections, urinary tract infections, increased risk of bone fractures (canagliflozin), euglycemic ketoacidosis, and necrotizing fasciitis. Canagliflozin also has a black box warning for a two-fold increased risk of lower limb amputation.
Thiazolidinediones (TZDs): pioglitazone, rosiglitazone
TZDs activate nuclear transcription factor PPAR-γ, resulting in increased insulin sensitivity. Both drugs are contraindicated in patients with class III-IV heart failure due to black box warnings for increased risk of heart failure. Rosiglitazone has a second black box warning for increased risk of myocardial events. Other adverse effects that may limit utility in practice include weight gain, edema, and increased risk of fractures.
Dipeptidyl peptidase-4 (DPP-4) Inhibitors: sitagliptin, saxagliptin, alogliptin, linagliptin
Gliptins stimulate insulin release and decrease hepatic glucose production. Mild adverse effects include headache and upper respiratory infections. Serious adverse effects include acute pancreatitis, urinary tract infections, extremity/back pain or osteoarthritis (with sitagliptin only). Gliptins do not have cardiovascular benefits and may increase risk of hospitalization for heart failure.
Meglitinides: repaglinide, nateglinide
Meglitinides, similar to sulfonylureas, stimulate insulin secretion by pancreatic beta cells. This means patients may develop tolerance to these medications over time, as seen with sulfonylureas. Meglitinides, unlike sulfonylureas, have a short duration of action and primarily affect postprandial glucose level. This means patients should be instructed to take meglitinides before meals, up to three times per day. Repaglinide has similar glycated hemoglobin A1C lowering abilities and hypoglycemia risk to sulfonylureas while nateglinide is not as good at lowering A1C but provides a lower risk of hypoglycemia.
Alpha-glucosidase Inhibitors: acarbose, miglitol
These drugs inhibit intestinal alpha glucosidase, preventing the breakdown of carbohydrates into simple sugars and ultimately resulting in lower postprandial blood glucose. Acarbose is generic and commonly used, however it is contraindicated in patients with the following: cirrhosis, colonic ulcers, intestinal disease or obstruction, inflammatory bowel disease, or diabetic ketoacidosis. The increased presence of carbohydrates within the intestines results in many of the GI side effects seen with this medication class.
Contributors: Dylan Smith, Kelly Karpa
Antihyperglycemics (2)- injectable
Currently there are 3 recognized classes of injectable antihyperglycemics.
Glucagon-like peptide-1 receptor agonists (GLP-1 RAs): liraglutide, exenatide
These medications mimic endogenous glucagon-like peptide-1 (GLP-1) resulting in a variety of effects: stimulation of insulin secretion, enhancement of insulin sensitivity (secondary to weight loss), slowing of gastric emptying, and endogenous glucose production. Liraglutide also reduces cardiovascular events and mortality for high-risk patients within 3-5 years. Nausea, vomiting, diarrhea, and hypersensitivity reactions are the most common adverse effects.
Amylin mimetics: pramlintide
Pramlintide is a synthetic analog of human amylin, inhibiting high glucagon secretion and reducing the rate of glucose absorption by slowing gastric emptying. This medication should only be considered for patients already receiving insulin for type I or II diabetes. There is a black box warning for severe hypoglycemia, so proper insulin adjustments should be made if initiating concomitant pramlintide. Contraindications for pramlintide include gastroparesis, drugs that stimulate gastrointestinal motility, poor compliance to insulin therapy or blood-glucose monitoring, or glycated hemoglobin (A1C) > 9%.
Insulin:
Endogenous insulin acts to move glucose out of the blood into the cells, resulting in decreased serum glucose levels. There are two groups of exogenous insulin used for hyperglycemia: human insulin and insulin analogues. Human insulins include isophane (NPH) insulin and regular insulin and analogues include insulin aspart, lispro, glulisine, detemir, and glargine. While human insulin is more affordable, insulin analogues act more similarly to endogenous insulin produced by the pancreas. The different types of insulin vary in their onset of action, the time to their peak effects, and the duration of action. The pharmacodynamic profiles of insulin and some clinical analogues are depicted below in a graph that is available from the Diabetes Education Online webpage for ‘Types of Insulin‘.
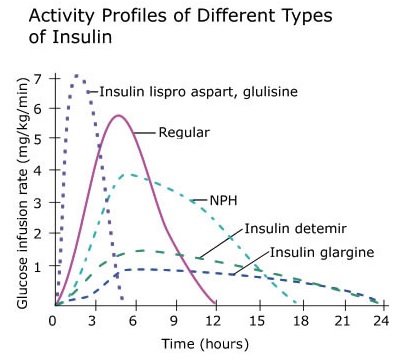
The longer-acting analogues, referred to as basal insulin, are used once or twice daily for continuous control of fasting glucose. Insulin analogues with a shorter duration of action, referred to as bolus insulin, are used to control spikes in blood glucose, especially following meals. A brief description of each type of insulin together with more information about the time course of effects of each can be found by searching Diabetes Education Online.
Contributors: Dylan Smith, Kelly Karpa
RESOURCES
This page provides access to a wealth of information about the drugs and therapies that are available for patients with type 1 diabetes. The information that is provided is suitable both for patients and early learners.
Drugs for hyperthyroidism
Thioamides, such as carbimazole and propylthiouracil, inhibit thyroid peroxidase and interfere with the formation of thyroid hormones. Carbimazole is a prodrug metabolised to the active metabolite thiamazole (also known as methimazole). As there are thyroid hormones stored in the thyroid gland, the onset of clinical action can vary from 3 to 12 weeks. Generally, carbimazole or thiamazole is preferred to propylthiouracil as it has a longer half-life and lower risk of hepatotoxicity. However, propylthiouracil has a faster onset of clinical action as it additionally inhibits the conversion of T4 to the more potent T3 and is therefore preferred for treating thyrotoxic crisis (or thyroid storm). Propylthiouracil is also preferred during the first trimester of pregnancy as it has a lower risk of teratogenicity. A rare (approximately 0.3 to 0.6 %) but potentially severe adverse effect of thioamides is agranulocytosis, which puts patients at risk of opportunistic infections. Therefore periodic blood counts are required, and patients must be warned to report any signs of infection (e.g., sore throat or fever). Fortunately, the agranulocytosis is reversible on thioamide withdrawal.
Iodides at high concentrations activate the Wolff-Chaikoff effect, an autoregulatory phenomenon suppressing thyroid hormone synthesis and the release of thyroid hormones. Formulations include Lugol’s solution, consisting of 5 % iodine and 10 % potassium iodide or potassium iodide tablets or saturated solution. Due to the suppression of thyroid hormone release, the onset of clinical action occurs within 24 to 48 hours and achieves a peak effect after 10 to15 days of continuous therapy. Because of the rapid onset of action, iodides are useful in the treatment of thyrotoxic crisis. Iodides can decrease thyroid gland size and vascularity when given over 1 to 2 weeks and so are also helpful before surgical thyroidectomy. However, the effect is not maintained when the iodide is discontinued. As iodide is required for thyroid hormone synthesis, when the gland “escapes” from the iodide block, it may produce severe exacerbations of thyrotoxicosis.
Radioiodine (131I) can be used for pharmacological thyroidectomy. Following oral administration, the radioiodine is rapidly concentrated in the thyroid gland, minimising exposure of the rest of the body to the radioactivity. 131I has a radioactivity half-life of 8 days and emits β particles and γ rays. The destructive β particles do not penetrate far and so destroy the thyroid gland with no detectable damage to surrounding tissues. However, the time course of the cytotoxic effect is slow, and it takes 2 to 3 months for the symptoms of hyperthyroidism to abate.
Drugs used for the management of thyrotoxic crisis include propylthiouracil, iodides, colestyramine, beta-blockers, corticosteroids and paracetamol. Propylthiouracil and iodides are used to suppress thyroid hormone production but are preferred to carbimazole or its active metabolite thiamazole because they have a faster onset of action as they inhibit the conversion of T4 to T3 and, in the case of iodides, the release of thyroid hormones. As thyroid hormones undergo enterohepatic recycling, being released in bile and reabsorbed in the small intestine, the bile-salt binding resin colestyramine can reduce plasma thyroid hormone levels during thyrotoxic crisis. Propranolol is a beta-blocker used to reduce the cardiovascular risk of acute hyperthyroidism. Although it is a nonselective beta-blocker, it is preferred for treating hyperthyroidism as it additionally reduces the conversion of T4 to the more potent T3. Corticosteroids, such as hydrocortisone (cortisol) or dexamethasone, are used to control systemic effects, including the risk of adrenal suppression and fever. Paracetamol is also used as an antipyretic.
RESOURCES
This links to the PubMed page for a review article that was published in 2016.
Drugs for hypothyroidism
Levothyroxine is a synthetic form of the thyroid hormone thyroxine (T4). Levothyroxine is commonly used for oral replacement therapy in the treatment of hypothyroidism. It has poor and variable oral bioavailability (40% to 80%) that can be decreased by age, foods, and certain drugs. Typically it should be taken with water only on an empty stomach 30 minutes to one hour before food, one hour before taking food, soya milk, coffee or bulk-forming laxatives (dietary fibre), and four hours before iron or calcium supplements or antacids. Levothryoxine is converted to the more potent triiodothyronine (T3) by deiodinases in the liver, kidney, and various target tissues and organs. It has a long half-life of 6 to 8 days, so it takes several weeks to reach steady-state plasma concentration. When administered orally, it has an onset of action in 3 to 5 days and must be taken consistently for 3 to 4 weeks before the peak clinical effect is achieved. The major adverse effects are due to the risk of hyperthyroidism on overdose. Risks include cardiac arrest, hypertension, palpitations, tachycardia, anxiety, heat intolerance, hyperactivity, insomnia, irritability, and weight loss. Long-term use of high doses has been associated with increased bone resorption and reduced bone mineral density, especially in post-menopausal women.
Liothyronine is a synthetic form of the thyroid hormone triiodothyronine (T3). Liothyronine is administered intravenously and orally for the treatment of myxoedema. Compared to levothyroxine, it has better oral bioavailability (approximately 95%), which is less strongly impacted by food and drugs, and a much faster onset of clinical action (2 to 4 hours) and time to peak therapeutic effect (typically 2 to 3 days). The faster onset of action is an advantage over levothyroxine in treating myxoedema. However, liothyronine is less desirable for chronic replacement therapy than levothyroxine as it is more potent and therefore has a greater risk of the cardiovascular adverse effects associated with thyroid hormone excess. Oral liothyronine is also sometimes used in combination with levothyroxine for chronic replacement therapy in patients with persistent complaints impacting their quality of life after levothyroxine alone. However, the benefits and long-term safety of combination replacement therapy remain inconclusive.
RESOURCES
This is a review article that was published in 2022.

This is a website run by the University of California, San Francisco. It has a wealth of information about diabetes and the medications and therapies that can be used to manage the condition, much of which is suitable for patients and early learners.