HIV type 1 (HIV-1, HIV) infects CD4+ T cells of the immune system, via interactions with CD4 on T cell membranes and with the co-receptors CXCR4 and CCR5, which are two chemokine GPCRs. Once inside the cell the HIV genome is inserted into the host genome and hijacks the host transcriptional and translational machinery to replicate new viral particles. HIV infection ultimately leads to destruction of CD4+ T cells as the T cells lyse and release new virus, which go on to infect and destroy more T cells. The cumulative effect dramatically reduces the patient’s T cell population and therefore their ability to mount an effective response to further infections.
Treatment with anti-HIV medicines (antiretrovirals or ARVs) is called antiretroviral therapy (ART). The principal action of ART is to lower viral load and promote immune re-constitution and viraemic control, with the aim of reducing the risk of progression to AIDS.
The ART drugs available target crucial and amenable steps in the life cycle of HIV infection and replication (see figure below). The FDA has approved more than two dozen antiretroviral drugs to treat HIV infection. A patient's initial HIV regimen generally includes three HIV medicines from at least two of the different drug classes described below.

Nucleoside/Nucleotide Reverse Transcriptase Inhibitors (NRTIs)
NRTIs inhibit activity of reverse transcriptase, a viral DNA polymerase that is required for replication of HIV and other retroviruses. Viral reverse transcriptase copies the single stand of the HIV’s RNA genome creating a double-stranded viral DNA that is able to integrate into the host chromosomal DNA. Host transcription and translation are hijacked to reproduce the virus. This group of drugs are analogues of the host’s endogenous deoxynucleotides that are required to synthesize viral DNA, but when incorporated in to a growing DNA molecule they block further elongation, acting as chain terminators. Drugs of this type can be either nucleoside or nucleotide analogues, with the former requiring kinase-mediated phosphorylation to generate active triphosphate molecules. Nucleoside reverse transcriptase inhibitors were the first type of ART drugs to be developed.
Examples include:
Abacavir, or ABC (Ziagen)
Didanosine, or ddl (Videx)
Emtricitabine, or FTC (Emtriva)
Lamivudine, or 3TC (Epivir)
Stavudine, or d4T (Zerit)
Tenofovir, or TDF (Viread)
Zidovudine, or AZT or ZDV (Retrovir)
Non-nucleoside Reverse Transcriptase Inhibitors (NNRTIs)
NNRTIs bind directly to the viral reverse transcriptase and inhibit its activity. This action prevents viral replication.
Delavirdine (Rescriptor)
Efavirenz (Sustiva)
Etravirine (Intelence)
Nevirapine (Viramune)
Rilpivirine (Edurant)
Protease Inhibitors (PIs)
HIV protease inhibitors are peptidomimetics that competitively inhibit the action of the virus aspartyl protease, and enzyme crucial for the proteolytic cleavage of nascent polypeptide precursors into mature viral proteins.
Atazanavir, or ATV (Reyataz)
Darunavir, or DRV (Prezista)
Fosamprenavir, or FPV (Lexiva)
Indinavir, or IDV (Crixivan)
Lopinavir + ritonavir, or LPV/r (Kaletra)
Nelfinavir, or NFV (Viracept)
Ritonavir, or RTV (Norvir)
Saquinavir, or SQV (Invirase)
Tipranavir, or TPV (Aptivus)
Cobicistat (Tybost) is an adjuvant drug that increases atazanavir and darunavir efficacy, but it can cause life-threatening kidney problems if it is adminstered with certain other medicines.
Atazanavir + cobicistat, or ATV/COBI (Evotaz)
Darunavir + cobicistat, or DRV/COBI (Prezcobix)
These first three groups of drugs work at the level of the HIV infected cell to inhibit viral replication.
The next groups of drugs have different mechanisms of action.
Entry (or Fusion) Inhibitors
Drugs of this class block viral fusion and entry to the T cells.
Enfuvirtide, or ENF or T-20 (Fuzeon), is a biomimetic peptide that binds to the viral transmembrane protein gp41, and inhibits formation of the entry pore that is required for the capsid of the virus to enter the cell. Enfuvirtide is active against HIV-1, with very low activity against HIV-2. Enfuvirtide is delivered by injection, so adherence may be an issue for some patients.
In March 2018, the US FDA approved a first-in-class treatment for heavily treatment-experienced patients with multidrug resistant HIV. Ibalizumab-uiyk (proprietary name Trogarzo; IMGT link) is an anti-CD4 (CXCR4) monoclonal antibody that inhibits the viral entry process (see Jacobson et al. (2009)), and is able to block CCR5- and CXCR4-tropic viruses. Ibalizumab-uiyk is to be used in combination with an optimized background regimen of other antiretroviral drugs.
CCR5 Antagonist
Drugs with this action are also entry inhibitors, but with a distinct mechanism of action compared to enfuvirtide. The CCR5 chemokine receptor is an important co-receptor that HIV-1 uses to attach to cells before viral fusion and entry into host cells. Maraviroc (MVC, Selzentry) is a CCR5 antagonist that inhibits the HIV-CCR5 interaction and thereby prevents HIV from entering the cells. Many treatment-experienced patients may have non-CCR5-tropic virus. Thus, screening patients with tropism assays (e.g., Trofile) before maraviroc initiation is essential.
Integrase Inhibitors (or integrase strand transfer inhibitors (INSTIs))
Integrase is a key viral enzyme that facilitates integration of retroviral DNA into the host cell genome. Drugs of this family inhibit this process, thereby preventing viral replication.
Dolutegravir (Tivicay)
Elvitegravir (Vitekta)
Raltegravir (Isentress)
Cabotegravir (Vocabria)
Attachment Inhibitors
This new class of HIV drugs blocks viral attachment to the host CD4 molecule on T-lymphocytes.
Fostemsavir was the first example of this class to be approved by the FDA (in 2020). It is indicated for HIV infections that cannot be successfully treated with other ARTs because of resistance, intolerance or safety considerations.
Capsid Inhibitors
Drugs with this mechanism of action block capsid protein oligomerization and disrupt interactions with host factors that are crucial for both early and late phases of the viral replication cycle. Lenacapavir was the first drug of this class to be approved for clinical use (in 2022, by the EMA & FDA). It is a long-acting drug that's administered as a subcutaneous depot injection, once every 6 months. It is prescribed in combination with other antiretrovirals. Like Fostemsavir, lenacapavir's use is reserved for HIV infections that cannot be successfully treated with other ARTs because of resistance, intolerance or safety considerations.
Fixed-Dose combination HIV medications
Abacavir + dolutegravir + lamivudine, or ABC/DTG/3TC (Triumeq)
Abacavir + lamivudine, or ABC/3TC (Epzicom)
Abacavir + lamivudine + zidovudine, or ABC/3TC/ZDV (Trizivir)
Efavirenz + emtricitabine + tenofovir, or EFV/FTC/TDF (Atripla, Tribuss)
Elvitegravir + cobicistat + emtricitabine + tenofovir, or EVG/COBI/FTC/TAF or ECF/TAF (Genvoya)
Elvitegravir + cobicistat + emtricitabine + tenofovir, or EVG/COBI/FTC/TDF or ECF/TDF (Stribild)
Emtricitabine + rilpivirine + tenofovir, or FTC/RPV/TAF (Odefsey)
Emtricitabine + rilpivirine + tenofovir, or FTC/RPV/TDF (Complera)
Emtricitabine + tenofovir, or TAF/FTC (Descovy)
Emtricitabine + tenofovir, or TDF/FTC (Truvada)
Lamivudine + zidovudine, or 3TC/ZDV (Combivir)
Cabotegravir + rilpivirine (Cabenuva; co-packaged) is a once monthly injectable regimen for uncomplicated infections.
ART adherence is essential to prevent drug-resistant strains of HIV developing. If ART is used properly HIV-positive patients can now live long, active lives.
Prescribing decisions are reached by considering existing medical conditions, immune system function, and should involve discussions about which regimen the patient would prefer, and would be most likely to adhere to.
Pre-exposure prophylaxis (or PrEP) is the most recent advance in ART, with the approval of Truvada as a therapy to reduce the likelihood of HIV infection in high risk individuals (e.g. to reduce the risk of HIV-negative people getting HIV from a sexual or injection-drug-using partner who is HIV-positive). The CDC (https://www.cdc.gov/hiv/basics/prep.html) reported that among people who inject drugs, PrEP reduces infection risk by >70%. If combined with ‘safe sex’ the risk of getting sexually transmitted HIV whilst taking PrEP is reduced by up to 90%.
Continuing care
CD4 count (every 3-6 months)
Viral load (every 3-4 months)
HIV strain tests to ensure a resistant form hasn’t appeared that would stop drugs from being effective.
Cholesterol and triglyceride tests, because HIV and many of the antiretroviral drugs that treat it can raise the levels of these fats
Checks for infections including STIs, and opportunistic infections such as pneumonia, Salmonella, candidiasis, hepatitis, tuberculosis and toxoplasmosis.
Ensuring vaccinations are up to date to prevent diseases such as chicken pox, measles, mumps, influenza, and polio. HIV positive patients can receive anti- pneumonia vaccines.
Ongoing Drug Development
Drugs with alternative modes of action are being sought to overcome the problems associated with acquired drug-resistance.
For example, PRO 140 is a humanized monoclonal antibody targeted against the CCR5 receptor. In Phase 3 clinical trial.
The infographic below presents a timeline of HIV drug approvals by the US FDA (https://hivinfo.nih.gov/understanding-hiv/infographics/fda-approval-hiv-medicines)


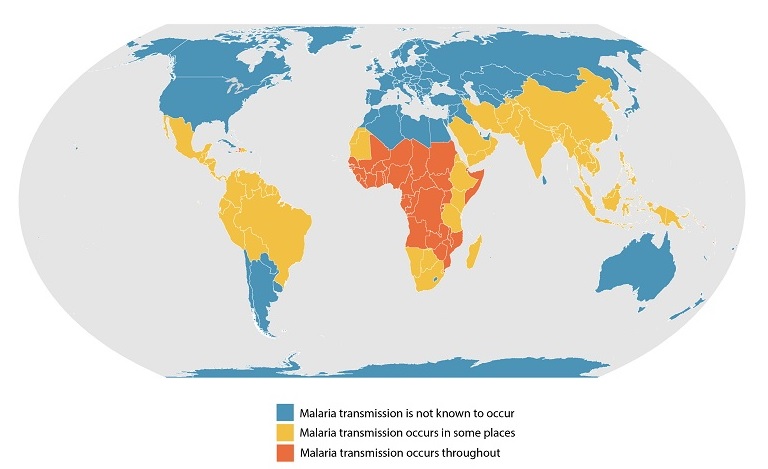



This webpage provides information about the species of Plasmodium that are recognised as causing malaria in humans around the globe. It is regularly updated.